Introduction
Probiotics and gut microbiota are two crucial elements in maintaining digestive health.
Probiotics are live microorganisms that provide health benefits, especially to intestinal health, when consumed in adequate amounts. Meanwhile, the gut microbiota refers to the diverse community of microorganisms residing in our intestines, playing a vital role in digestion and immune function
.
Maintaining a healthy gut is essential for overall well-being. A balanced gut microbiota supports proper digestion, strengthens immune responses, and helps prevent diseases. Imbalances can lead to various health issues, including metabolic disorders and gastrointestinal conditions.
This article explores the relationship between probiotics and the gut microbiota in intestinal health and disease prevention. You will learn how probiotics contribute to maintaining intestinal health and their potential therapeutic roles in preventing or managing diseases. By understanding these dynamics, you can use probiotics for better digestive health.
Understanding Probiotics and How They Work
Probiotics are defined as live microorganisms that provide significant health benefits when consumed in adequate amounts. These beneficial microbes predominantly belong to specific strains such as Bifidobacterium and Lactobacillus, which are renowned for their positive effects on gut health.
Common Probiotic Strains and Their Impact
Here are some common probiotic strains and their impact on gut health:
- Bifidobacterium: Known for enhancing the balance of the gut microbiota, this strain helps in breaking down complex carbohydrates and producing essential vitamins. Its presence is crucial in maintaining a healthy digestive tract.
- Lactobacillus: Often found in yogurt and other fermented foods, this strain aids in lactose digestion and helps prevent infections by producing lactic acid, which creates an inhospitable environment for harmful bacteria.
How Probiotics Support Gut Health
Probiotics contribute to gut health through several mechanisms:
- Blocking Pathogen Entry: By occupying niches within the intestinal tract, probiotics can physically block pathogens from adhering to the gut lining, reducing the chance of infections.
- Maintaining Mucus Barrier Integrity: Probiotics support the production of mucus, a protective layer that shields the intestinal walls from harmful substances and microbes. This mucus barrier is crucial for preventing pathogen infiltration and maintaining gut health.
- Producing Antimicrobial Substances: Certain probiotic strains produce antimicrobial compounds such as bacteriocins and hydrogen peroxide. These substances have natural antibiotic properties that help neutralize pathogenic bacteria.
These mechanisms highlight how probiotics not only contribute to digestive wellness but also play a vital role in safeguarding against intestinal disorders. Each strain offers unique benefits, reinforcing why incorporating probiotics into your diet can be advantageous for maintaining a balanced gut microbiota.
The Gut Microbiota: A Key Player in Digestive Health and Disease
The gut microbiota consists of diverse microbial communities that reside in our intestines, playing a crucial role in maintaining digestive health. These communities are made up of trillions of bacteria, viruses, fungi, and other microorganisms that live together in harmony within the human gut. Each person’s microbiota is unique, influenced by factors such as genetics, diet, and environment.
Why a Balanced Gut Microbiota Matters
A balanced gut microbiota is essential for:
- Proper Digestion: Microbes help break down complex carbohydrates and fibers that the human body cannot digest on its own.
- Immune Function: By interacting with immune cells, the microbiota helps train and regulate immune responses.
- Disease Prevention: A healthy microbial balance protects against harmful organisms and reduces the risk of certain diseases.
The Consequences of Dysbiosis
When this delicate balance is disrupted, it leads to a condition called dysbiosis, which can have serious consequences. Dysbiosis is linked to increased vulnerability to infections due to weakened barriers against harmful organisms. Inflammatory conditions such as Crohn’s disease and ulcerative colitis are also associated with an imbalanced microbiome. This imbalance may contribute to chronic inflammation in the gut, worsening these conditions.
Moreover, dysbiosis has been connected to more severe outcomes like colorectal cancer. The altered composition of microorganisms can result in higher production of harmful substances and inflammatory signals that promote cancer development.
Probiotics: A Solution for Dysbiosis
Probiotics play a vital role in addressing dysbiosis by restoring microbial balance. They help replenish beneficial bacteria, such as those from the Bifidobacterium and Lactobacillus genera, which are often reduced during dysbiotic states. These probiotics assist in maintaining the integrity of the intestinal barrier and reducing inflammation, offering a therapeutic approach for conditions like antibiotic-associated diarrhea (AAD) and inflammatory bowel disease (IBD).
Understanding how probiotics interact with the gut microbiota is crucial for developing strategies to improve intestinal health and prevent diseases related to imbalances in microorganisms.
Probiotics as a Treatment for Intestinal Disorders
Clinical trials have provided substantial evidence supporting the role of probiotics in preventing and managing intestinal disorders. One notable example is their effectiveness in addressing antibiotic-associated diarrhea (AAD). Antibiotics, while essential for combating bacterial infections, often disrupt the delicate balance of the gut microbiota, leading to AAD. Studies indicate that certain probiotic strains can replenish beneficial bacteria, thereby reducing the incidence and severity of this condition.
In the context of inflammatory bowel disease (IBD), which includes conditions like Crohn’s disease and ulcerative colitis, probiotics have shown promise. Clinical trials have demonstrated that specific strains such as Bifidobacterium and Lactobacillus can enhance gut health by modulating immune responses and promoting anti-inflammatory effects. These probiotics contribute to restoring microbial balance, alleviating symptoms, and improving patient outcomes.
The potential benefits of probiotics go beyond just these two conditions. Ongoing research continues to explore their wider uses in gastrointestinal health, highlighting their significance not only as a preventive measure but also as an additional treatment in various intestinal diseases. The dynamic relationship between probiotics and the gut microbiota plays a crucial role in maintaining intestinal health and preventing disease progression.
The Role of Probiotics in Modulating Immune Responses and Reducing Inflammation
Understanding how probiotics influence immune responses is crucial for appreciating their role in maintaining gut health. These beneficial microorganisms interact with the immune system to promote a balanced response, essential for preventing excessive inflammation and ensuring intestinal wellness.
Probiotic Actions on the Immune System:
- Probiotics can enhance the activity of regulatory T-cells, which play a pivotal role in controlling immune responses.
- They stimulate the production of anti-inflammatory cytokines while decreasing pro-inflammatory ones, aiding in a harmonious immune environment.
The potential for inflammation reduction by probiotics is particularly noteworthy in managing conditions like Crohn’s disease and ulcerative colitis. These chronic inflammatory disorders benefit from the anti-inflammatory mechanisms offered by probiotics.
Mechanisms in Inflammatory Conditions:
- Certain probiotic strains produce short-chain fatty acids (SCFAs), such as butyrate, which possess anti-inflammatory properties.
- By fortifying the gut lining and enhancing mucus production, probiotics help prevent harmful bacteria from triggering inflammation.
Incorporating probiotics into your routine may offer significant benefits for those dealing with inflammation-related intestinal issues. Their ability to modulate immune responses highlights their therapeutic potential beyond digestion, pointing to a broader impact on overall health.
Exploring the Potential Link Between Probiotics, Gut Microbiota Alterations, and Colorectal Cancer Prevention
The relationship between probiotics and gut microbiota is gaining interest for its potential in preventing colorectal cancer. New evidence suggests that certain probiotic strains may have protective effects against colorectal cancer by influencing the gut microbiota.
Key Insights:
- Modulation of Gut Microbiota: Probiotics like Lactobacillus and Bifidobacterium are known to influence the composition and function of gut microbiota. These changes can create a healthier microbial environment, which is important in reducing cancer risks.
- Production of Short-Chain Fatty Acids (SCFAs): Certain probiotic strains increase the production of SCFAs such as butyrate. These compounds have been shown to have anti-inflammatory effects and may stop cancer cells from growing in the colon.
- Reduction of Carcinogenic Compounds: Probiotics can lower levels of harmful enzymes and carcinogenic substances in the gut, potentially decreasing cancer risk.
These insights highlight the potential role of probiotics in promoting gut health and possibly reducing the occurrence of colorectal cancer. While research is still ongoing, these findings open up opportunities to explore probiotics as an additional method in cancer prevention strategies.
Considerations for Probiotic Use: Risks, Limitations, and Future Directions
While the benefits of probiotics are well-documented, it is essential to consider the potential risks associated with their use. Excessive consumption of probiotics can lead to adverse effects such as bacteremia, where bacteria enter the bloodstream and may cause serious health issues.
Certain populations are more susceptible to these risks. Individuals with compromised immune systems, including those undergoing chemotherapy or living with autoimmune diseases, may face heightened vulnerability. Similarly, patients undergoing invasive medical procedures or those with pre-existing conditions affecting their gut health should exercise caution.
Key considerations include:
- Overuse Risks: Over-reliance on probiotics without professional guidance can disrupt the natural balance of the gut microbiota.
- Vulnerable Populations: Extra care is needed for individuals with weakened immune defenses or those recovering from surgery.
Future research should focus on delineating safe consumption levels and identifying specific strains that pose minimal risk to vulnerable groups. Understanding these factors will enhance the therapeutic application of probiotics in promoting gut health while minimizing potential adverse effects. This knowledge is vital for optimizing their role in maintaining intestinal wellness amidst an expanding landscape of probiotic products.
Conclusion: Embracing Probiotics as Allies for a Healthy Gut
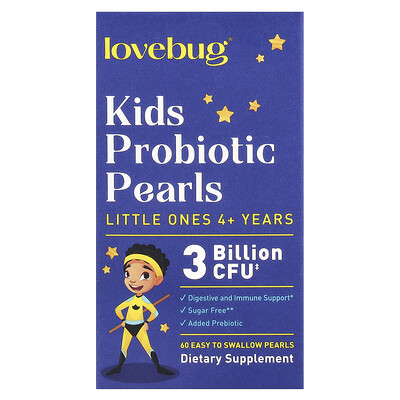
Incorporating probiotics into your daily routine can significantly boost digestive wellness. Consider adding probiotic-rich foods such as:
- Yogurt
- Kefir
- Sauerkraut
Alternatively, high-quality probiotic supplements offer a convenient option.
Exploring the full potential of probiotics in promoting gut health and preventing intestinal diseases remains an exciting frontier. Ongoing research is essential to uncover new insights into how probiotics and the gut microbiota in intestinal health and disease can transform our understanding of digestive wellness.
Embrace probiotics as allies in your journey towards a healthier gut and overall well-being.
Discover more from NatureZen Market
Subscribe to get the latest posts sent to your email.